|
Deactivation
of a demand pacemaker by transurethral electrocautery. Wajszczuk WJ,
Mowry FM, Dugan NL. The New England journal of medicine.
1969 Jan; 280(1):34-5.
Journal code: 0255562. ISSN: 0028-4793. L-ISSN: 0028-4793.
http://chemport.cas.org/cgi-bin/sdcgi?APP=ftslink&action=reflink&origin=springer&version=1.0&coi=
1%3ASTN%3A280%3ADyaF1M%252FktVGjsw%253D%253D&md5=c8ba02e6b084a27f393aa7788cf3ae7c
Electromechanical suppression of a demand
pacemaker associated with electrode perforation.
Rubenfire M,
Timmis H,
Freed P,
Evangelista JL,
Ginsberg H,
Wajszczuk WJ.Journal
of electrocardiology. 1973;
6(4):367-71.
http://www.labmeeting.com/paper/14345524/rubenfire-1973-electromechanical-suppression-of-a-demand-pacemaker-associated-with-electrode-perforation
Implication of a persistent left superior
vena cava in transvenous pacemaker therapy and cardiac hemodynamic
monitoring.
Rubenfire M,
Evangelista J,
Wajszczuk WJ,
Kantrowitz A. Chest.
1974 Feb; 65(2):145-7.
http://chestjournal.chestpubs.org/content/65/2/145.long
An anomalous persistent left superior vena cava may complicate the
insertion of transvenous pacemaker electrode catheters as well as the
catheterization of the pulmonary artery. It
is important to recognize the anomaly because of the ease of
confusing the position of the catheters passing through the
coronary sinus into a distal coronary vein
rather than the right ventricular apex. If the condition is known and
is associated with a patent right superior vena cava, a catheter or
electrode should probably be passed from the right side. If this is
not possible, our experience indicates that the flow-directed
balloon-tipped catheter (Swan-Ganz) can be passed easily without
fluoroscopic control through an anomalous
left superior vena cava to the pulmonary artery. Using a similar
balloon-tipped flow-directed pacemaker electrode may be helpful in its
positioning in the apex of the right ventricle.
While short-term temporary pacing via the
coronary sinus is probably acceptable, placement of a permanent
electrode in the coronary sinus is dangerous. If there is congenital
absence of the right superior vena cava, an epicardial
electrode is likely preferred.
Analysis of pacemaker
pulse-wave shape. Basic principles and simulated study of
malfunction. Waldemar J. Wajszczuk and
Joseph K. Cywinski. Bulletin,
Sinai Hospital of Detroit.
Vol. 23, No 1, January 1975.
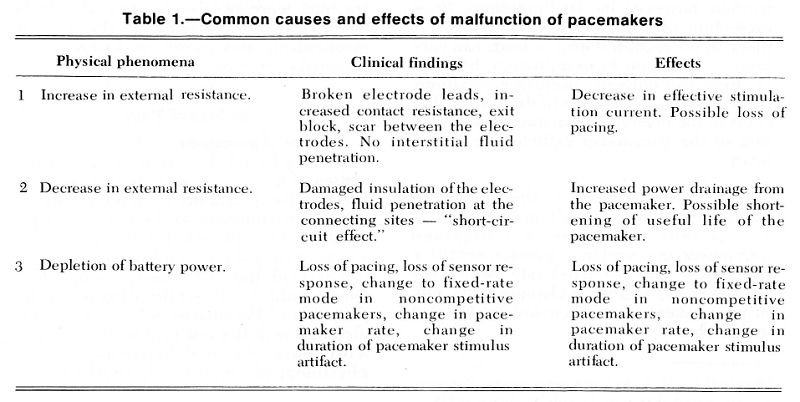
Summary and Conclusion
Recent rapid growth of a network of the Pacemaker Follow-up Clinics
created a demand for development of the diagnostic criteria to improve
the differentiation between their continuing normal function and their
potential malfunctions, either related to age (battery depletion) and
to other early malfunction. This experimental study was designed to
evaluate the importance of oscilloscopic analysis of the pacemaker
pulse-wave shape in follow-up of performance of the implanted
pacemaker and in evaluation of the causes of its malfunction or
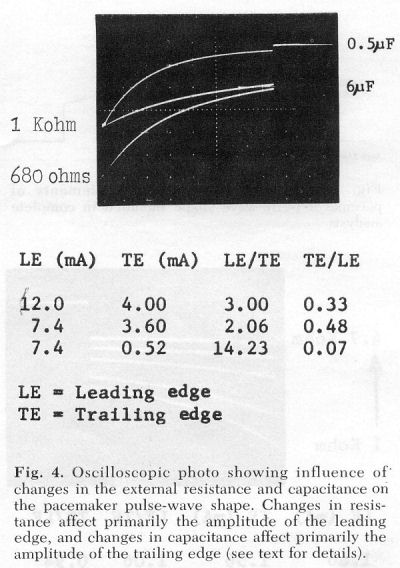
failure. Specially constructed artificial test loads provided the
possibility of reproducing a variety of abnormal clinical conditions
which included changes in resistance and capacitance of the
pacemaker-electrode-myocardium circuit. Differentiation was made
between clinical conditions associated with penetration of the
interstitial fluid and situations with damage of the electrodes but
without penetration of the fluid.
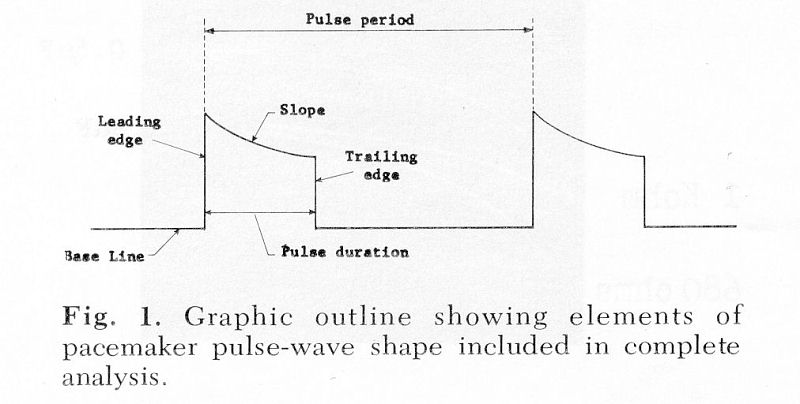
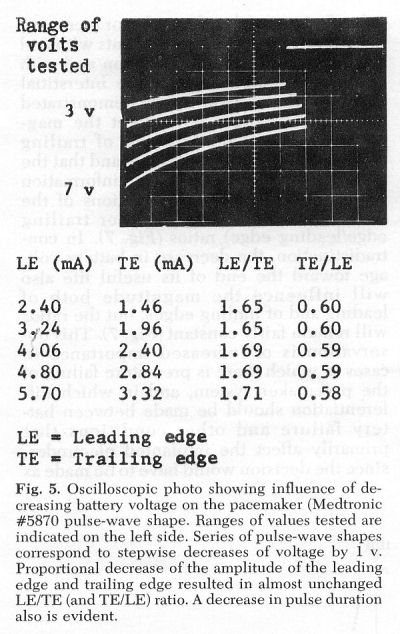
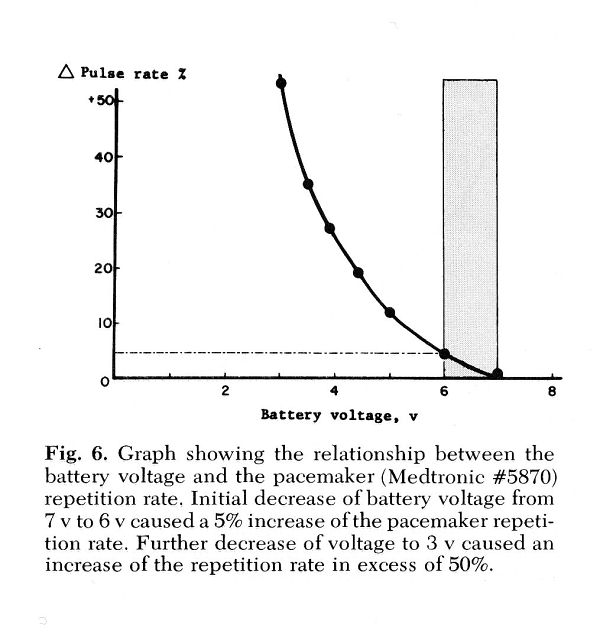
The examples of pacemaker pulse-wave shapes presented in this paper
were obtained using a Medtronic pacemaker, Type 5870. Elements of
evaluation included measurements of pulse duration, pulse period
(pacemaker repetition rate), and amplitudes of the leading edge (LE)
and trailing edge (TE) of the pacemaker pulse-wave shape. Calculations
of the LE/TE and TE/LE ratio proved extremely important and valuable.
This ratio allowed differentiation between:
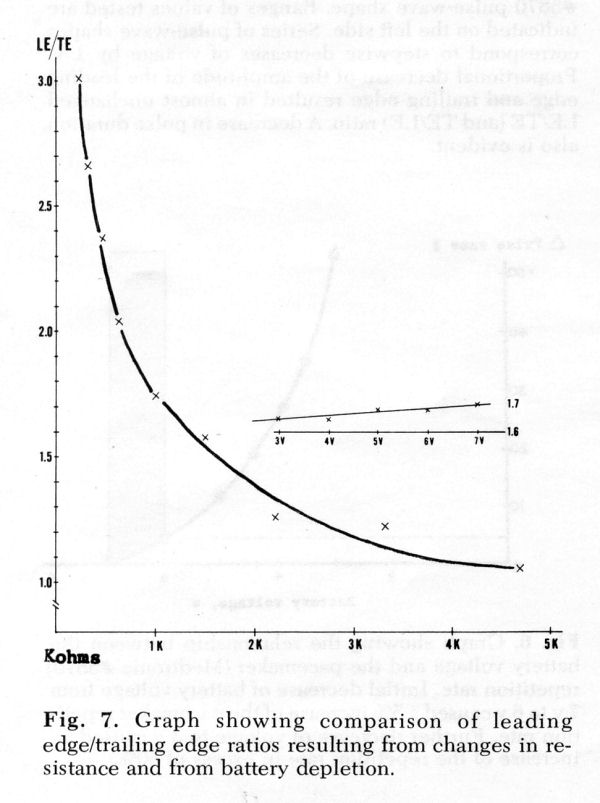
A. Malfunction of the pacemaker system due to increased resistance
(broken electrode, "exit block," etc.) and the depletion of the
batteries;
B. Increased resistance without and with penetration of the
interstitial fluid (damage of the insulation causing changes in
the capacitance).
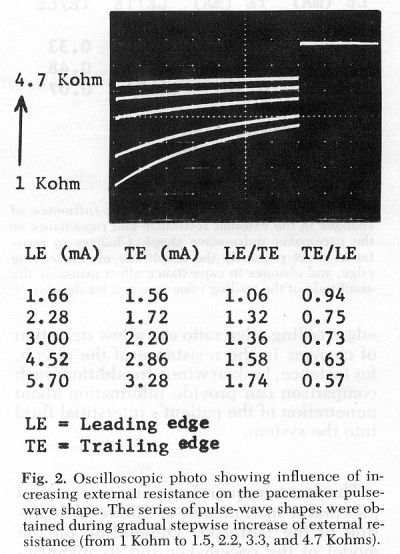
- Gradual increases of resistance caused
disproportionate decrease of the amplitudes of LE and TE and
produced marked gradual decrease of the LE/TE ratio.
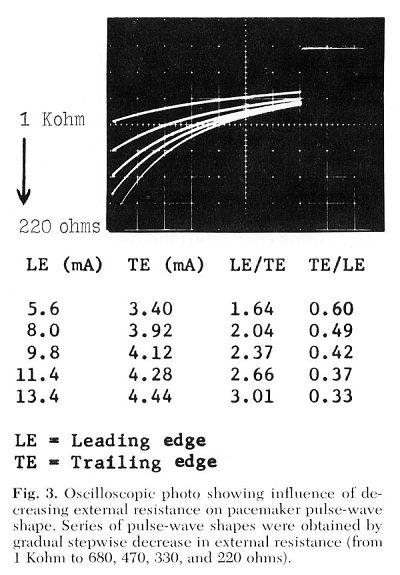
- Increased capacitance affected primarily the
amplitude of the TE out of proportion to that of the LE and
resulted in a sudden and marked change in the LE/TE ratio.
- Decrease of the battery voltage did not
affect the LE/TE ratio to a significant degree. These findings
proved to be helpful in differentiating between premature failure
or malfunction of the pacemaker system due to battery depletion and
that due to other causes such as breakage of the electrode or "exit
block."
The importance of the pacemaker pulse-wave shape evaluation in
differentiation of the causes of its malfunction or failure was well
documented. The provided series of pacemaker pulse-wave shapes can be
used as guidelines in evaluating the performance of the pacemaker.
| Increasing
External Resistance
|
Decreasing
External Resistance
|
| Changes in Ext.
Resistance and Capacitance
|
Decreasing
Battery Voltage
 |
Abstracts and Presentations:
-
Simulated diagnostic patterns of artificial cardiac pacemaker failure;
experimental study. Presented at the Fifth Annual Meeting of the
Association for the Advancement of Medical Instrumentation, Boston,
Massachusetts, March 23-25, 1970
-
Importance of oscilloscopic analysis of pacemaker pulse waveshape in
pacemaker follow-up. (Abstract). Wajszczuk, Waldemar J.
and Joseph K. Cywinski, Medical Instrumentation 7: 83, 1973
|