|
Clinical
Publications
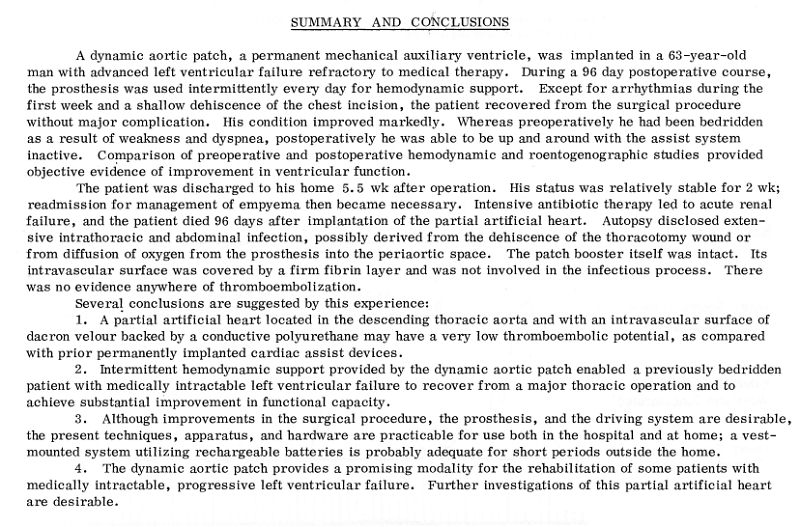
Initial Clinical Experience
with a New Permanent Mechanical Auxiliary Ventricle: The Dynamic
Aortic Patch. Kantrowitz, Adrian, Joseph
S. Krakauer, Melvyn Rubenfire, Dov Jaron, Paul S. Freed, W. Welkowitz,
Philip N. Cascade, Waldemar J. Wajszczuk, Marc Lipsius, M.
Ciborski, Steven J. Phillips, and M. T. Hayden. Transactions -
American Society for Artificial Internal Organs 18
(1972): 159-167
http://echo.gmu.edu/bionics/goldvol.htm
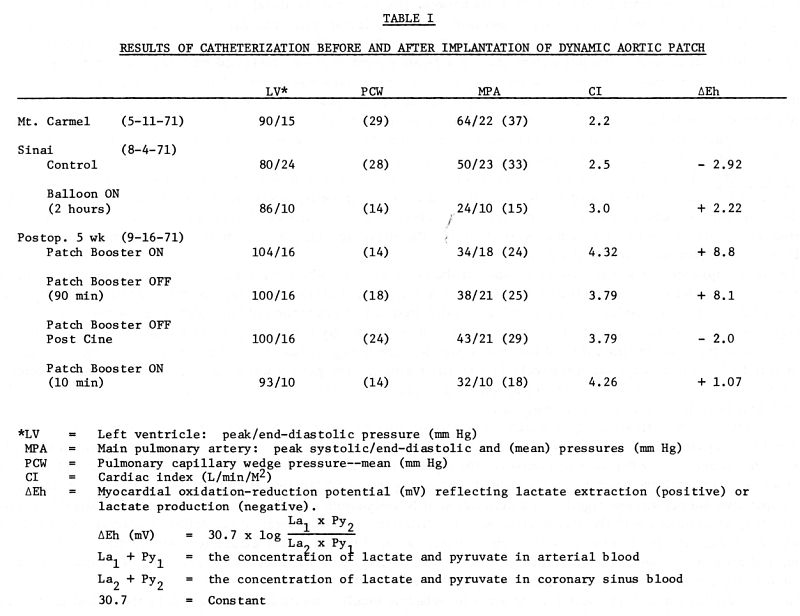
Treatment of Cardiogenic
shock by Intraaortic Balloon Pumping. Results in 42 patients.
A. Aris, J. Krakauer, S. Phillips, M. Ciborski,
W .J. Wajszczuk, M. Rubenfire, Dov Jaron and A. Kantrowitz..
Actas del VI Congreso Europeo de Cardiologia, Madrid, Spain, 1972,
(Published by Editorial Paz Montalvo, Madrid, pp. 971-972,
1974).
Balloon pump treatment
reversed the shock in 39 (93%) of the 42 patients. Of these, 27 (64%)
regained circulatory stabilization allowing discontinuation of
treatment and removal of the balloon. Fifteen (36%) died during
treatment. Of the 27 patients regaining circulatory stabilization, 12
(28%) recovered completely and were discharged from the hospital. The
causes of death among the 30 non-survivors included myocardial rupture
in 13 patients.
The results suggest that
this method of circulatory support is effective in treatment of
patients in cardiogenic shock. Furthermore, the simplicity and safety
as well as the hemodynamic effectiveness of this therapeutic modality
indicates that balloon pumping may have potential role in other
applications: 1) Support before, during and after cardiac
surgery. 2) Improved myocardial perfusion for angina
pectoris. 3) Circulatory support during coronary angiography or
vetriculography. 4) Prolonged term support in chronic left
ventricular failure.
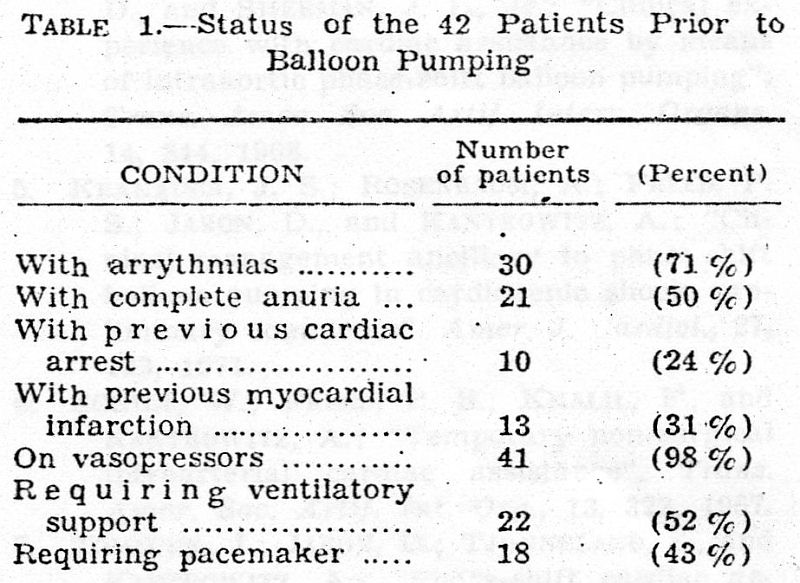
Intra-aortic phase-shift balloon
pumping. Clinical applications.
Aris A, Krakauer J, Phillips SJ, Ciborski MG, Rubenfire M,
Wajszczuk WJ, Kantrowitz A.
J Cardiovasc Surg
(Torino).
1973; Spec No: 647-50.
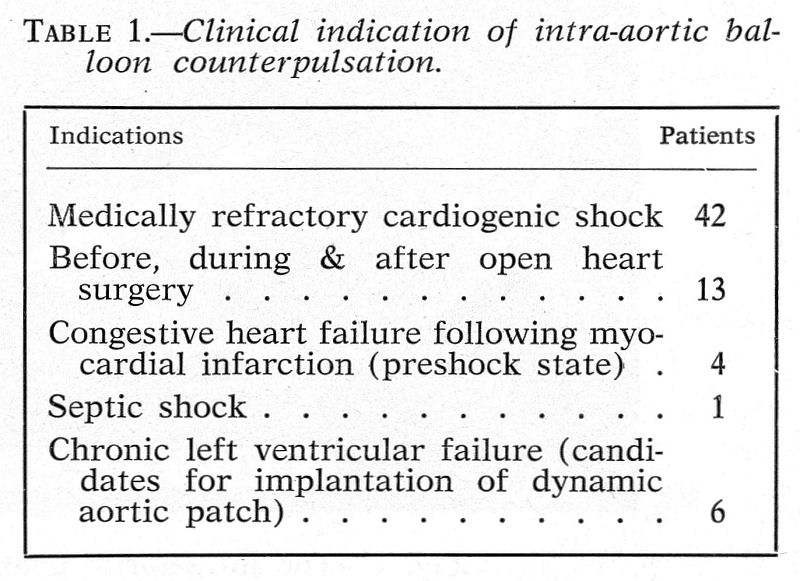
Optimum results
have been obtained in medically refractory cardiogenic shock.
Sixty-six patients were treated with the intra-aortic counterpulsating
balloon for the indications listed above. Shock was reversed in 39
(93%) of the 42 patients, and in 27 (64%) the resulting hemodynamic
stabilization permitted the procedure to be discontinued. Twelve
patients (28%) were discharged from the hospital.
Peri-operative support (open heart surgery) included: 5 high-risk
patients with severe bi-ventricular failure, who were pumped
pre-operatively and post-operatively, all showed hemodynamic
improvement, 3 survived the procedures and 2 were discharged from the
hospital; six patients were unable to be “weaned” from cardiopulmonary
bypass - after insertion of the balloon, 4 were able to be taken of
the bypass but only 1 was a long-term survivor.
Late post-operative complications developed in 2 patients. One of them
with cardiac tamponade, sternal dehiscence and profound shock,
underwent re-exploration under continuous balloon pumping. He
recovered and was discharged from the hospital. The other patient
experienced multiple hepatic and circulatory complications resulting
in severe metabolic imbalance that culminated in death.
Severe congestive heart failure was treated in 4 patients. Two showed
initially hemodynamic improvement but died 48 and 72 hours after
initiation of pumping. The other 2 were pumped, at first continuously,
later intermittently, for 35 days without deleterious effects despite
the duration of pumping.
In 1 patient with gram-negative septicemia complicated by shock,
pumping was ineffective and the patient succumbed.
Six patients in terminal chronic left ventricular failure underwent
balloon pumping to evaluate their hemodynamic response in
consideration of implantation of a permanent device. Two of them
showed a good response and subsequently underwent successful
implantation procedure.
Results indicate that balloon pumping is an effective form of
temporary circulatory support in a variety of clinical situations
involving left ventricular failure.
Current indications for mechanical circulatory
assistance on the basis of experience
with 104 patients.
Wajszczuk WJ, Krakauer J, Rubenfire M, Ciborsky M, Malinowski E,
Kantrowitz A: (abstr) Am J Cardiol 33: 176, 1974
Neurological Abnormalities
in the Leg(s) After Use of Intraaortic Balloon Pump.
Honet, Joseph C., Waldemar J. Wajszczuk, Melvyn Rubenfire,
Adrian Kantrowitz, and James A. Raikes. Archives of Physical
Medicine and Rehabilitation 56, (August 1975): 346-352.
http://www.labmeeting.com/papers/author/wajszczuk-w
Six patients from a group
of 39 who survived after treatment with the intraaortic balloon pump
(lABP) had significant neurological deficits in one or both legs
associated with the use of the lABP. The device was used in a group of
89 patients initially for cardiogenic shock but its use has been
expanded for patients having the following conditions: preshock;
severe congestive heart failure; refractory angina; and for those
undergoing open-heart surgery. The six patients who had neurological
sequelae had eight lABP insertions into the thoracic aorta through the
femoral artery and had neurological abnormalities and/or
electromyographic abnormalities in nine lower extremities ranging from
a foot drop to almost total paralysis of the lower extremity. The
pathophysiology of the neurological deficit is postulated to be an
obstruction to blood flow, or thromboemboli, in the femoral artery.
Patient Selection for Cardiac Surgery in Left
Ventricular Power Failure. Philip N.
Cascade, MD; Waldemar J. Wajszczuk, MD; Melvyn Rubenfire, MD;
Stewart E. Pursel, MD; Adrian Kantrowitz, MD. Arch Surg 110
(11):1363-1367, 1975
http://profiles.nlm.nih.gov/GN/B/B/D/K/_/gnbbdk.pdf
PAPER READ BEFORE THE 23RD SCIENTIFIC MEETING OF THE INTERNATIONAL
CARDIOVASCULAR SOCIETY, BOSTON, JUNE 19-20, 1975
http://archsurg.highwire.org/cgi/content/abstract/110/11/1363
Nineteen patients in acute left
ventricular power failure following acute myocardial infarction were
given support with intraaortic balloon pumping and underwent cardiac
catheterization. Hemodynamic response to diastolic augmentation,
results of left ventriculography, and observations of selective
coronary arteriography were evaluated to determine which patients
could survive without operation, which would require operation to
survive, and which could be predicted not to survive operation. Of ten
patients who underwent operation, three were long-term survivors. Two
patients predicted to have a good prognosis without surgery did
survive. Of three patients who had been determined to require
operation but not undergo it, two died in the hospital and one a month
later. The four patients whose conditions were considered inoperable
died in the hospital. The results indicate that current methods of
predicting the need for corrective surgery are relatively accurate and
that the rate of survival in surgically treated patients may be
increased.
Physiologic and angiographic
evaluation of severe left ventricular power failure to determine
feasibility of cardiac surgery.
Proceedings;
Cascade PN, Wajszczuk WJ, Rubenfire M, Pursel S, Kantrowitz A.
J Cardiovasc Surg (Torino).
1976 Jan-Feb;17(1):88.
THE CHEST X-RAY IN ACUTE LEFT VENTRICULAR POWER
FAILURE:
AN AID TO DETERMINING PROGNOSIS OF PATIENTS
SUPPORTED BY
INTRAAORTIC BALLOON PUMPING.
PHILIP N. CASCADE, ADRIAN KANTROWITZ, WALDEMAR J. WAJSZCZUK AND MELVYN
RUBENFIRE.
Am JRoentgenol
116:1147-1154, 1976
Serial chest x-rays were used as a means of
evaluating the hemodynamic status of 43 patients in acute left
ventricular power failure (LVPF) complicating acute myocardial
infarction who were assisted with balloon pumping. The following
findings were reported:
1. In patients with acute myocardial infarction,
prediction of the hemodynamic status on the basis of chest x-rays is
less reliable when severe LVPF is present as a complication.
2. The incidence and severity of roentgenographic
findings of congestive heart failure and pulmonary edema are increased
in patients with severe LVPF compared to patients with uncomplicated
myocardial infarction.
3. Improvement in the roentgenographic degree of
heart failure with positive clinical and hemodynamic responses to 24
hr or less of balloon pumping is an indication that patients in
severe acute LVPF may survive. Patients with deteriorating or
unchanging chest x-ray findings have an extremely poor prognosis.
These patients should be evaluated by cardiac catheterization and
coronary arteriography to determine the appropriateness of emergency
surgical correction.
Intraaortic Balloon
Pumping 1967 Through 1982: Analysis of
Complications in 733 Patients.
Kantrowitz, Adrian, Tarik Wasfie, Paul S. Freed, Melvyn Rubenfire,
Waldemar J. Wajszczuk, and M. Anthony Schork. The
American Journal of Cardiology 57 (15 April 1986): 976-983
http://www.labmeeting.com/papers/author/wajszczuk-w
Between June 1967 and
December 1982, 872 attempts at intraaortic balloon pumping (IABP) were
made in 733 patients. Nearly 75% of the patients were men; the
proportion of women has increased in recent years. The principal
indication for IABP support initially was cardiogenic shock, but over
the years, preoperative support, weaning from cardiopulmonary bypass
and unstable angina have become the primary indications. Complications
of IABP were classified and distributed by severity (minor: I [15%]
and II [26%]; major: III [3%] and IV [1%]) and type ([vascular [22%],
infectious [22%], and bleeding [7%]). Vascular complication rates were
higher in women (32 vs 18%; p = 0.0001), in diabetic patients (32 vs
20%, p = 0.003), and in hypertensive patients (27 vs 20%, p = 0.02).
These did not vary with the duration of IABP support (range of
duration 0 to 76 days). The rate of infectious complications was
related to location where IABP was performed (coronary care unit 26%,
operating room 12%). The rate of fever and bacteremia increased
significantly with duration of IABP support, but the rate of local
wound infection did not. In conclusion, most IABP complications are
minor, resolve after balloon removal, are related to vascular status
of the patient and, with the exception of bacteremia, are independent
of IABP duration.
Risks associated with
intraaortic balloon pumping in patients with and without diabetes
mellitus. Wasfie, T : Freed, P S : Rubenfire, M :
Wajszczuk, W : Reimann, P : Brozyna, W : Schork, M A : Kozlowski,
J : Kantrowitz, A. Am-J-Cardiol. 1988 Mar 1;
61(8): 558-62
http://grande.nal.usda.gov/ibids/index.php?mode2=detail&origin=ibids_references&therow=269401
http://www.labmeeting.com/papers/author/wajszczuk-w
Between 1967 and 1982,
intraaortic balloon pumping (IABP) was attempted in 733 patients. Of
these, 132 were diabetic: 51 patients were managed with diet alone, 46
patients took oral hypoglycemic agents and 35 patients required
insulin. Vascular complications associated with IABP occurred in 34%
of the insulin-dependent diabetics, in 18% of other diabetics and in
14% of nondiabetic patients. Infectious complications were 37, 22 and
25%, respectively. Seventy-five diabetic patients (57%) were
discharged alive from the hospital after balloon pumping, essentially
the same proportion as among nondiabetic patients (58%). It is
concluded that although diabetics incur a higher complication rate,
IABP is not contraindicated. |